Table of Contents
What is Exocrine Pancreatic Insufficiency (EPI)?
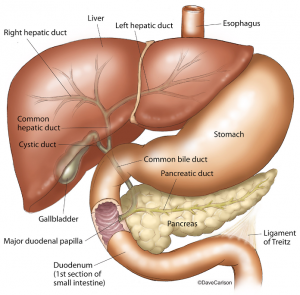
EPI –when the pancreas does not secrete enough digestive enzymes– is common in people with chronic pancreatitis. This is because as the pancreas gets scarred, the part of the pancreas that generates enzymes is destroyed and thus is unable to produce these enzymes that are essential in the digestive process.
Leading causes of EPI:
- Chronic pancreatitis: 15-30% prevalence
- Pancreatic restriction/older age: 15-40% prevalence
- Cystic fibrosis: 80-90% of CF patients
- All infants up to 6 months of age!
What happens if you have Exocrine Pancreatic Insufficiency or EPI?
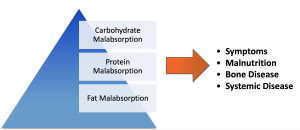
EPI causes 4 main problems:
- Carbohydrates are not properly absorbed
- Proteins are not properly absorbed
- Fats are not properly absorbed
- This can lead to malnutrition
Signs and symptoms of Exocrine Pancreatic Insufficiency
- Steatorrhea: Pale oily stools and “sticking” phenomenon.
- Abdominal Symptoms: Like diarrhea, bloating, abdominal pain, and gas.
- Fat-soluble vitamin deficiency (A, D, E, K):
- Rashes and, night blindness → Vitamin A deficiency.
- Metabolic bone disease → Vitamin D deficiency.
- Hemolytic anemia, neuropathy, retinopathy → Vitamin E deficiency.
- Bruising/bleeding →Vitamin K deficiency.
How do doctors diagnose Exocrine Pancreatic Insufficiency or EPI?
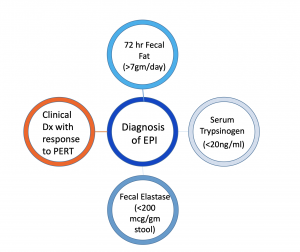 Doctors usually diagnose EPI using a fecal elastase test. Elastase is an enzyme made by the pancreas that helps down essential nutrients like fats, proteins, and carbohydrates after you eat. If little or no elastase is found in the stool, it might mean the enzyme is not working properly and thus your doctor might diagnose you with Exocrine Pancreatic Insufficiency. In adults, pancreatic insufficiency is often a sign of chronic pancreatitis.
Doctors usually diagnose EPI using a fecal elastase test. Elastase is an enzyme made by the pancreas that helps down essential nutrients like fats, proteins, and carbohydrates after you eat. If little or no elastase is found in the stool, it might mean the enzyme is not working properly and thus your doctor might diagnose you with Exocrine Pancreatic Insufficiency. In adults, pancreatic insufficiency is often a sign of chronic pancreatitis.
Sometimes a doctor can prescribe Pancreatic Enzyme Replacement Therapy (PERT) and see if you respond to pancreatic enzymes. If you do, that can help them diagnose you.
What are pancreatic enzyme pills? What do they do?
Pancreatic Enzymes (also called Pancreatic Enzyme Replacement Therapy or PERT) are extracts from pig pancreas given as a pill that you take with your meal. They can be enteric-coated or “non-enteric-coated.” They result in improved protein and fat absorption and reduced symptoms in children and adults with EPI. Their intended purpose is to mimic the function of the pancreas during the process of digestion.
Risks associated with PERTs
High-dose PERT is associated with fibrosing colonopathy. A eheoretical viral transmission, i.e. if the pig from which the pancreas was extracted was infected with a virus and infected the patient, is unlikely. PERTs contain purines, which can be a risk for patients with gout, renal impairment, and hyperuricemia. Current research is focused on developing microbial/recombinant-based PERTs.
How do you take PERTs?
Determine the correct amount
Infants should take around 4,000 units per every 4 oz formula or breast milk
Children less than 4 years old should take 1,000 units per kg per every meal, or 500 units per kg per snack.
Adult and/or Child 4 years and older: 500 units per kg per meal, 250 units per kg per snack
Dosing should not exceed 2,500 lipase units per kg of body weight per meal or 10,000 lipase units per kg of body weight per day. For example, for a 60 kg (132-pound) adult, 6 Creon capsules (24,000 units) per meal is recommended. This table is a general guide to PERT dosing based on weight, which is how the FDA approved it. Pancreatologists suggest that dosing should consider exocrine pancreatic function and the amount of fat consumed. Consult with your pancreatic specialist for the dose that is right for you.
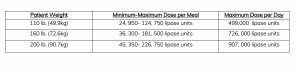
Examples of Weight-Based Dosing of PERT
When to take enzymes
Take with the first bite of a meal. Consider adding more during and towards the end of the meal, especially if the meal is longer than twenty minutes. The goal is to mimic the effects of your pancreas in relation to the quantity of food and type of fats. The dose should be adjusted to the fat content and size of the meal.
Hydration/Alkaline pH
Ensure adequate hydration. Patients with Cystic Fibrosis have impaired and bicarbonate/fluid production, which makes this even more necessary. Consider adding an acid blocker.
Side effects
If the PERT is not absorbed it will produce minimal side effects. Older PERT formulations are associated with elevated uric acid levels (gout) in Cystic Fibrosis patients.
Challenges to taking pancreatic enzymes correctly
There are many barriers to taking PERT therapy as directed. It is a lifelong therapeutic commitment that involves a large quantity of capsules. Additionally, patients might forget to time their doses with a meal. Patients might also struggle with depression or inadequate coping mechanisms. Poor adherence to PERT therapy is more problematic among patients during adolescence and into young adulthood. Young women, in particular, may resist taking full doses due to fears of gaining weight and may have a distorted body image.
It is important that patients and family members understand that this is a required lifelong therapy. Patients should self-monitor their progress in order to improve their compliance with the treatment. If possible, they should follow CF Foundation recommendations.
Care providers must understand the importance of effective communication with patients going through PERT therapy. They should have respectful and forthright conversations with their patients and gauge their compliance with therapy, particularly during life transitions. An interdisciplinary approach is also important, so, if necessary, service providers should suggest counseling with nutritionist colleague(s).
Use of PERTs for chronic pancreatitis pain
Only Viokace, which exists only in quick release form, may help reduce chronic pancreatitis pain. Other PERTs have shown NOT to be effective for pain, although they are effective for enzyme insufficiency.
This drug has worked best in young women without a dilated pancreatic duct on CT or MRI scans. A normal dose is three tablets (20,880 lipase units) with each meal with an acid blocker. The mechanism works to prevent stimulation of the pancreas in response to a meal.

Dr. Steven Freedman, MD, Ph.D. Director, Pancreas Center, Beth Israel Deaconess Medical Center, Chief of the Division of Translational Research, and Professor of Medicine, Harvard Medical School
The information and graphics on this page come from the Busting the Myths about Pancreatic Enzymes webinar, organized by Mission: Cure. The webinar addresses the facts (and myths) about Exocrine Pancreatic Insufficiency (EPI) and pancreatic enzymes.
